08/18/2020
Cathy Ryan loves discussing fascia and its relation to bodywork. Her practice and hands-on work have been shaped by related research. Today, her advice is to slow down and lighten up pressure. In this podcast, Cathy talks about her scar tissue management and understanding the process of facilitating change to new and mature tissue after insult.

This episode sponsored by Anatomy Trains and Yomassage.
00:00 Kristin Coverly: Yomassage is now offering ABMP podcast listeners $100 off their 25-hour certification from now until September 1st with the code ABMP 100. Don't miss this opportunity to take advantage of the biggest discount Yomassage has ever offered. Yomassage is revolutionizing the wellness industry by combining therapeutic touch, mindfulness and restorative stretch. Take your career to the next level and become a certified Yomassage therapist. Learn more at yomassage.com.
[music]
00:44 Darren Buford: Welcome to The ABMP Podcast. My name is Darren Buford. I'm the Editor-in-Chief of Massage & Bodywork magazine and Senior Director of Communications for ABMP. I'm joined by my co-host Kristin Coverly, licensed massage therapist and Director of Professional Education for ABMP. Our goal is to connect with luminaries and experts in and around the massage, bodywork and wellness profession in order to talk about the topics, trends and techniques that affect our listener's practices.
01:16 DB: Our guest today is Cathy Ryan. Cathy is a CMTBC registered massage therapist with an interest in patient-centered care, evidence-informed practices and lifelong learning. She is engaged in the profession in a variety of clinical, educational and leadership capacities over the past 30 plus years. An established continuing education instructor, Cathy has presented at conferences internationally and in the areas of scar tissue management and myofascial pain and dysfunction, which also constitute her clinical practice focus. She has written numerous articles, featured in various industry publications, co-authored Traumatic Scar Tissue Management, and is a chapter contributor in Fascia, Function and Medical Applications and Oncology Massage.
02:00 DB: Cathy is also the co-host of the podcast Massage Therapy without Borders. And Cathy Ryan's article, "Scar tissue, not breakable but changeable" was our cover story for the July August 2020 issue of Massage & Bodywork magazine. And we just recently added a three-part webinar series with Cathy on scar tissue management in the ABMP Education Center at abmp.com/ce. Hello friend.
02:24 Cathy Ryan: Hey, so lovely to see the two of you again.
02:28 KC: Hi Cathy, welcome.
02:30 CR: Thank you so much.
02:33 DB: So how...
02:33 CR: And wow, luminary, whoo.
02:35 DB: Yes. Luminary. You're a luminary.
02:37 CR: I'm not... Well... [chuckle]
02:38 DB: We're gonna put you in that category.
02:40 CR: Thank you so much.
02:41 DB: That bio alone, my goodness, I'm intimidated already before the conversation begins.
02:46 CR: Oh no.
02:48 DB: Okay, so tell us a little bit about your background and what brought you to massage therapy.
02:52 CR: Well, born a science nerd so I figured I would probably at some point end up in healthcare, my mom and two of her sisters were nurses, so I know that that had some influence, massage therapy, specifically, what took me in that direction is a sport injury that I had in my early 20s that I had had prior and I saw a massage therapist and was just blown away at how more quickly I recovered from that injury than I had previously. So I was working and saving money so I could go back to school and eventually found my way to a massage therapy school.
03:32 KC: I love it. So now let's pick up the thread, we're in massage, you're deep diving into that world, you're loving it. How did your specific interests/fascination/passion for fascia begin?
03:47 CR: Really early on, one of my massage therapy instructors in massage therapy school back in the late '80s had done the training at the Guild for Structural Integration. So he started to talk about this mysterious tissue called fascia because back then there was literally nothing other than a few plates and Netter or Gray's Anatomy, but there really wasn't much conversation happening in manual therapy about fascia as a contributor to human movement, and in practice, I found that the massage therapy training that I had was very good and my patients were really appreciating the work, but there were certain things that people were coming in with where I found that the sustainability just wasn't there.
04:37 CR: So back in the day, when I went to school, Travell, the big red books were the... Called the bible, were sort of it in the day, so doing a lot of trigger point work at that time in sort of the typical fashion that we were trained to do, poke your thumb in there, whatever, and it felt good in the moment for folks, but two weeks later, they'd come back and would be the same thing all over again so I just wasn't satisfied with the sustainability. One of my philosophies to care is I do my best to work myself out of a job, so it sent me searching for, "Okay, what's missing here, what else could I be doing to help my folks coming into my practice have more sustainable outcomes." And fascia just kinda stuck with me from when my teacher was talking a bit about it, so I started to scramble to look for whatever I could. And as I mentioned, there wasn't much.
05:39 CR: So pretty early on, I came across old VHS tapes of Michael Shea, who's a long-time Rolfer and then eventually Tom Myers' work and then in the early 2000s, I discovered Robert Schleip's website and then my science brain completely exploded at that point, and then eventually on to the Fascia Research Congress.
06:08 KC: Fantastic. Cathy, how do you describe this mysterious tissue called fascia?
06:15 CR: It really depends. It depends on context. So in terms of like... There's the classic definition that's changing, it's very fluid coming out of the research congress, so if I'm talking to my colleagues, we talk about it in that context, but in my practice, it really does depend upon who the person is that I'm talking to and what their issue is and how I describe it and its role, and perhaps how it's contributing to what's going on for them. I think one of the more common ways that I talk about it is, for example, I'll give you a classic example. In my practice, some woman comes in and says, "My hamstrings are really tight and I've been stretching and stretching and stretching, and they just... Nothing's happening. Why are my hamstrings so tight?" And so I try to describe to them, "Well, sometimes it's not necessarily a linear issue, so the hamstring may not be in a shortened position. Maybe it's just being squeezed by this bag that surround it, or perhaps it's not sliding inside the bag that surround it."
07:28 CR: So I'll describe fascia more in its role, its function in our body, what it does in terms of facilitating movement or impeding movement as the case may be. What I found over the years is some of the... Both in my practice that it's easiest to convey what this tissue does in it's vastness are folks who are hunters 'cause they butcher their own animals, and I apologize to anyone if I'm offending them, 'cause they've seen it, they've had their hands on this issue and they can see how it's connecting the calf muscle to the back of the leg on up the chain, so it's really easy to describe its global... The global concept of fascia to people who have seen it in the body of animals.
08:20 KC: Yeah. And I really like the idea of having a few different ways to describe fascia in the back of your mind, because many of us as therapists are a little bit stumped when a client asks, "We're gonna do some mild fascia release." "What's that? What's fascia?" [laughter] There's a moment of pause, like, "How do I take this big concept to bring it down into the moment in words that they can understand?" So I think that's really helpful to give a few examples, but also for us as therapists to have a few of those in the back of our minds. It's great. I'm gonna pick up on one word that you used in that description, and you used the word "sliding". Can you tell us a little bit more about what you mean when you reference "sliding" with fascia?
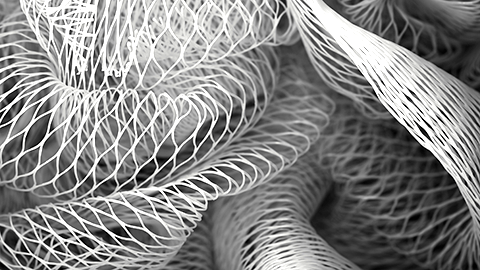
09:00 CR: Yeah. And this is a fairly new concept for us to think about and incorporate into the work that we're doing. And for me, that aha moment about the whole sliding thing was at the very first Fascia Congress. And it was Dr. Guimberteau's presentation, when he showed the endoscopic video that he had. It was the first time we had seen what this looks like in the human body. And I think most of us probably remember Gil Hedley's The Fuzz Speech, and all this fibril network, and when we don't move at all, gloms together, and then lo and behold, if you have a live human form with fluid in there, that network looks very different and it's not actually sticking things together, it's just part of that loose-connective tissue network that serves the sliding function.
09:54 CR: So when, usually back in the day when I went to school, it was all about levers and muscular contraction, and certain muscles have to stretch over a joint for movement to happen, but we now understand that that movement is much more complex in that, and that various chunks or layers of tissue have to slide in reference to one another in order for a movement happen. And that includes at a very superficial level too, 'cause oftentimes we think movement is joint, deeper tissues, but movement is also about skin, superficial fascia, and the ability for at that level, layers to slide in order for movement to be able to happen.
10:40 KC: And I know from working with you that you're really excited about a lot of the research that's been done about fascia. There's been some incredible findings. How does the information that we learn from those research studies inform how we as therapists understand and work with fascia?
10:56 CR: Well, and I think Guimberteau's work for me was a perfect example of how that research informed my hands, because his work in particular, and the Steccos' as well, got me thinking much more about the fluid environment and less about, let's say strands of fibers, which is much more... In massage therapy our training is very myocentric and all about the muscle fibers and stretching and contracting, and stretching and contracting. So much of the early myofascia work was about deforming tissue or stretching tissue to try to get length or space for things to move.
11:40 CR: And when I started to delve into Steccos' research and saw Guimberteau's stuff, it got me thinking about the fluid environment around the various chunks or fibers, and is that a changeable, essentially talking about ground substance, if it is a changeable fluid. So it can change from a very viscous or thick goo to something that is more conducive to creating space and allowing things to slide better. So looking at that research got me thinking about, "Okay, so if that softening that I feel under my hands when I'm working is not about, let's say a tension release mediated by the nervous system." So we think in terms of a muscle relaxing and dropping its tone, that may be happening, but there may be something else happening within that fluid environment that also constitute that change that happens underneath my hands." So it got me thinking about that.
12:39 CR: And thinking about how can I use my hands to better facilitate that. And I think one of the big changes that came for me was the amount of force or pressure that is needed to facilitate that kind of change. And also, some of Schleip's early work about the angle at which we go into the tissue. So reading that research has really changed my hands. I use my hands very differently today than I did 10 years ago, 15 years ago, and certainly 30 years ago.
13:09 KC: I love that phrase. Research has really changed my hands. That's fantastic. And I think listeners can tell already just this far into the podcast, that there's a huge depth of knowledge around fascia and how it applies to our work and ways to understand it, how much there is to understand. If a therapist said to you, Cathy, that's a lot of information. What are the most important things and aspects that I need to keep in mind when working with the fascia? How would you respond to them?
13:38 CR: Lighten up and slow down. Really, I think that is if we talk about the actual mechanics of my hands, that's what's changed the most is to lighten up and slow down. That has been the biggest change for me. And it would appear it has been a very productive change in my practice based upon the feedback that I'm getting from the people that I'm working with, and more sustainable change as well. So that really did fulfill what I initially went out looking for was how to achieve better outcomes for my patients. 'cause at the end of the day, that's really what it's all about for me.
14:18 DB: Let's take a short break to hear a word from our sponsors.
14:21 KC: Anatomy Trains, and the Laboratories of Anatomical Enlightenment, are excited to invite you to Dissection live stream, a regional and layered journey through the human body with Tom Myers and Todd Garcia. New dates coming soon. Student Jan Ball who attended the last Dissection says the whole live stream dissection course was truly a unique educational experience. It was profoundly moving. I gained so much from it, it was one of the most valuable educational opportunities that I've had. I'm truly grateful to Tom, Todd, and the whole team of people involved who made this unique opportunity available. This experience will be delivered through Zoom webinar with high-quality audio and video, multiple perspectives, and time for questions. Visit anatomytrains.com for dates and details.
15:13 DB: Now let's get back to the podcast.
15:16 KC: Let's bridge some information from topic to topic here a little bit. So we're gonna move from fascia in general as a conversation into scar tissue-specific aspects of fascia and working with clients. So I had the absolute pleasure to work with you and your teaching partner Nancy Keeney Smith, on a three-part webinar series for the ABMP Education Center on scar tissue management. So of course you were coming from the fascicle perspective, Nancy was coming from that lymphatic system perspective and how the two work together and are combined into what we need to think about and work with when working with a client with scar tissue, both aspects. What specific considerations do we need to keep in mind as therapists when we're working with scar tissue?
16:04 CR: It's not breakable would be the first thing that I would say. In the article, if you want me to come up swinging in a science nerd kinda way, come up to me and say, "Oh, Cathy, blah, blah, blah, breaking up down scar tissues?" No, we can't break this stuff. We're talking about collagen which has a tensile strength of steel. My hands are strong after 30 years, but they're not that strong. The other issue that I have with that in precision in language, is that unfortunately, I think it implies that we need to work with the tissue in a particular way to get it to break. So it implies that we need to be really assertive or aggressive with the tissue, and really to get the changes that we're looking for, it's just not necessary.
16:50 CR: And unfortunately, I think there's a safety component in that as well. And as well, it also has a comfort component in it for our patients. So if we can get the work done in a way that's not invasive, more comfortable, or receivable for the patient or the client, and it's safer, less potential for adverse events, then why wouldn't we? And it's physiologically implausible. And I think, unfortunately, in our profession in massage therapy, there are some of those things that continue to float around, like removing toxins and other things that make us look not very well informed if we're having conversations with... Interprofessionally So that's part of my issue with the breaking it thing. And then the other thing, I think what really... Nancy and I came together very serendipitously, Mary Law was the orchestrator of that at the International massage therapy research conference a number of years ago and got Nancy and I together and it was just such a fantastic opportunity for us to work together.
18:01 CR: But I think really one of the things that was the driver for the book was that in our conversations early on, both of us were saying, pretty much all of the scar tissue workshops that we see out there are after the fact, so how to work with this stuff months, years down the road, and both Nancy and I in our practice, our scar tissue work starts very early on. There are times depending upon the type of surgery and a number of other factors that I may be working with someone within a few days after surgery. And for us, it was really important to take that deep dive into wound healing science to really understand the process 'cause my thing has always been as a massage therapist if I understand process, I won't be stumped. I can always kind of figure out what I might be able to do to assist this person. So we took the deep dive into the wound healing process and how to work in the early stages to perhaps temper the overproduction of, let's say, not well-formed scar tissue.
19:08 CR: 'Cause anytime we injure ourself, we have scar tissue. We need that in order to get those squappy bits back together so our body can function. And we either end up with well-formed scar tissue that serves a good function or pathological or not well-formed scar tissue that's going to impede function. So for us it was how to work with this stuff in the very early stages. And that's where I think the lymphatic system and understanding the workings of the lymphatic system is very important in the early stages. In the very early stages, it's really about calming down the nervous system and making sure there's good flow. So and Nancy has been my lymphatic Marvin to help me. I had some lymphatic training but really she has been the one that has contributed significantly to my evolution of understanding of the lymphatic system for sure. Yeah, so in the early stages, I'm not really doing... It's usually about three to four weeks out before I would start doing what I would call direct scar tissue work, so working with the connect tissue, the fascia. So the early stages, it's the nervous system and the lymphatic system.
20:19 DB: What constitutes a mature scar?
20:22 CR: In the medical definition, they say that a scar is fully formed or mature at about one year out. So really it's about the stability of the new collagen that we have. So they say that the new collagen matures at about a year out, but scars continue to change, much like we can say that we mature at the age of 21. That's a lot questionable. [chuckle] We continue to mature over the course of our lifetime, hopefully. It's the same with scars. I've worked with so many people and I have a couple of scars myself that continue to change over 5, 10, 15, 20 years. But the technical or medical definition is they mature when the collagen is fully formed or sturdy enough that it's not going to be an issue.
21:17 DB: After an injury or an insult, what's causing the homogenous reconstruction of scars versus like a chaotic organization or fibrosis, is it random? Is it dependent upon the person or the insult?
21:29 CR: Oh, Darren you use sciencey words. Oh, it gets me all happy. [laughter] When we took the deep dive into the wound healing research essentially it boiled down to two things that can cause the process to go sideways. So there are things that can contribute to poor healing. Infection, I think is a very classic example of wounds that won't heal, while certain underlying health issues... So we know that people who have compromised circulatory systems may not heal a wound as well. But in terms of the overproduction of anomalous collagen, there are two primary drivers of that. And one is excessive or prolonged inflammation and the other is undue tension around the area that is healing. And I get really excited when I saw those things in the wound healing research, because those are two things that form excessive prolonged fluid in an area that just screamed out lymphatic work to me, and then unnecessary or undue tension. Well, it's like, okay, nobody's gonna take us to the map about can massage therapy impact tension in the tissues.
22:53 CR: I think anywhere we go, any interprofessional conversation, if we say massage therapy can impact tension in tissues, I think pretty much everybody's gonna go, "Yeah, of course, it is. Of course, it can." So I get really excited when I saw those things. So I was like, "yes." So even though I don't have specific research, those were pretty easy dots to connect that I think is pretty solid from a physiological possibility perspective. So it was a pretty reasonable nexus to connect those dots.
23:31 DB: When you're working with scar tissue is there a modality that works specifically better than another or is it like an all-encompassing management strategy?
23:42 CR: Understanding the stages of wound healing are really important 'cause as I mentioned in the very early stages, I'm working mostly... Let's say I'm using my hands in ways that will help facilitate changes in the... Guided by the lymphatic system and the nervous system. And then later on when it's, say, older scars, I'm gonna be using my hands in different ways. When I talked earlier about having some kind of impact on the fluid environment because it's not breakable, I'm not gonna be able to break it apart. So in order for, to restore, let's say, some loss of movement or function, one of the things that I potentially can do is to shift the fluid environment so there's better sliding in there and more space between the fibers so that they can do their job. Collagen turnover continues to happen. We're not born with a strand of collagen and that's a strand that we keep throughout our lifetime. The cells turnover all the time, and I think it was Tom Myers who talked about the shelf life of collagen being... I can't remember how many days. Approximately a year or something like that, a year and a half.
24:49 CR: So my thing is, is with, let's say, older scars, they're still potentially changeable. We can't break them but there still may be some change that can be facilitated. So we know that immobilization has a detrimental impact on tissue. So if we can use our hands to get this tissue more soft and pliable and the person can start to do movement themselves by virtue of how they're moving their body, their body will start to change that collagen, as its own natural process. So, if I can help a person start to move better themselves, by virtue of their own movement, they're going to facilitate changes going forward.
25:34 KC: That's great, Cathy. You've shared such great and in-depth information about scar tissue, and fascia, and lymph, and how we work with that. I think it's going to inform all of us, and change the way we look at and address our own scars, but also our clients' scars, as they come into our practice. So, incredibly helpful. Several times throughout the pod, you've referenced the International Fascia Research Congresses. So, can you tell us, for all of us fellow science nerds listening along, what are those congresses like? What happens, what's the buzz, how does it feel? What goes down?
26:09 CR: And not just because I'm a total fascia nerd, but it really is one of my favorite conferences to attend, for so many reasons. The atmosphere is just so collegial, and you have these hardcore research scientists and clinicians in the same room, which was... Now, it seems like, "Oh, okay." That happens more frequently, but in 2007, when that first congress happened, really had never kind of happened before, [chuckle] so it's just... And it was so fascinating to see these hardcore scientists engaged in conversation with clinicians. And many of us didn't have, let's say, the language that they have, scientifically, to discuss things. But they were just so jazzed by how jazzed we were [chuckle] about their work. And there were a number of them that went away... You know, after the fact, we heard various scientists talk about how having that kind of conversation with clinicians actually changed their research, or drove different research, because they got excited about the fact that this is really applicable.
27:21 CR: People are really using this stuff, it's really making a difference out there. Wow, that's so cool! I'm not just sitting down in this basement, pecking away at research because it interests me. Somebody is actually finding something exciting about this. And I would encourage any manual therapist to attend that conference, because it's got fascia in the title, but so much information has come out of that conference, about how our work works, for us to really start to understand mechanisms of action. And how our work works, and in understanding that at a deeper level. Again, it has changed my hands, because it's really got me thinking about, "Okay, if that makes this happen over here, how can I use my hands to get that to happen even more, or more consistently?" So, for me, it really helped shift to more consistently reliable outcomes. So, really, is a piece or not... But it's such an exciting... And again, it does have fascia in the title, but I think, as a manual therapist, I think it's one of the most important conferences for us to attend.
28:28 KC: And what's exciting is now, with everything that's happening in the world, and conferences are moving to a more virtual platform, there's a chance in the future that therapists all across the world will have a chance to participate and view some, if not all, of those congresses and conferences in the future, which I think is really exciting. Cathy, what are you excited about regarding the future of fascia research and massage therapy?
28:52 CR: Wow! Such a... I don't even know where to begin. I think one of the most exciting things for me has been... Is some of the visual stuff that has come from that conference. I'm a visual learner, so for me, I get really excited when I saw Guimberteau's work, 'cause it's the first time we'd ever seen how stuff slides around in there, [chuckle] in the living tissue, with the fluid still in there. And, as well, there's quite a bit of Helene Langevin, and Steccos', and a number of others, Pilat, and a group of researchers working with Pilat, over in Spain. A number of them are starting to use high-definition real-time ultrasound to show changes before and after treatment. And certainly Paul and Prendergast had that one that they did, but they showed the change in collagen density before and after skin rolling, which was like blew my mind. Someone who's doing scar tissue work, that was just like, "Oh" kind of moment for me. So, you know I don't necessarily have to see it to believe it, but having that visualization really made an impact on me. Like Langevin's work, where she showed malsliding in people with low back pain of the thoracolumbar fascia, and how that is potentially a contributor to both pain and dysfunction for low back patients. That made a huge impact on me, 'cause it really started to change how I was working with my low back pain patients.
30:21 KC: Important question, Cathy. Do you have an "I heart fascia" bumper sticker on your car?
[laughter]
30:28 CR: Ah, I wish! Where can I get one?
30:31 KC: We'll make that happen for you. Promise.
30:33 CR: I'm just gonna have, like 17 of them plastered all over our vehicle.
30:38 DB: We wanna thank our guest, Cathy Ryan, for joining us today. Cathy, where can listeners find out more information about you, the podcast. How can they connect with you?
30:49 CR: ABMP, for starters. I believe you have my email address posted along with the three-part series, Heal Well. Of course, my friends... My dear friends at Heal Well, and I've got a three-part... Sorry, a five-part explain fascia course available through their website, their learning management system. And, yeah, so email is probably the best way to get a hold of me. If folks are looking for me, if they are going to fascia conferences, likely I'll be there, either in person or virtually. So that's another way to... If you wanna chat with me, I'm gonna be doing a presentation for the Polish Fascia Symposium, October 2-4. So that's pretty exciting, too bad I don't get to go to Poland, but... Nice to be invited to do it virtually.
31:41 DB: That's right. Thank you so much, Cathy.
31:44 KC: Thanks so much for being here. Great information, Cathy.
31:47 CR: Oh, thank you so much. Always a pleasure to hang out with you guys.
[music]
31:55 Speaker 4: This has been a production of Associated Bodywork and Massage Professionals. ABMP is a leading association for massage therapists and bodywork professionals in the United States and beyond. From liability insurance to professional advocacy, award-winning publications to the world's largest continuing education library for massage, to this podcast, no organization provides more for its members and the profession than ABMP. ABMP works for you.
32:27 KC: Thank you for listening. If you haven't already done so, please subscribe to the ABMP Podcast on iTunes, Google Play, or wherever you find your favorite podcasts.





