10/28/2022
A massage therapist accidentally finds an electrical wire running down their client’s neck, alongside their sternocleidomastoid (SCM) — surprise! It turns out to be a deep brain stimulation (DBS) device to help treat Parkinson’s disease.
DBS can also be used to treat a handful of other conditions, and treating more conditions continues to be investigated. So the chance you could have a client with a DBS device is higher than ever. How do we do that safely? Listen to this episode of “I Have a Client Who . . . ” for more.
Resources:
Pocket Pathology: https://www.abmp.com/abmp-pocket-pathology-app
Image of Deep Brain Stimulation: https://commons.wikimedia.org/wiki/File:Deep_Brain_Stimulation.jpg
Deep Brain Stimulation (2021). Available at: https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/deep-brain-stimulation (Accessed: 26 October 2022).
Deep Brain Stimulation – Advantages, Risks and Conditions Treated (no date a). Available at: https://www.aans.org/ (Accessed: 25 October 2022).
Deep Brain Stimulation (DBS) FAQ | Boston Scientific (no date) www.dbsandme.com. Available at: https://www.dbsandme.com/en/support-and-resources/faq.html (Accessed: 26 October 2022).
Deep Brain Stimulation (DBS): What It Is, Purpose & Procedure (no date) Cleveland Clinic. Available at: https://my.clevelandclinic.org/health/treatments/21088-deep-brain-stimulation (Accessed: 26 October 2022).
Franchina, P. (2019) ‘Deep brain stimulation and swimming’, American Parkinson Disease Association, 4 December. Available at: https://www.apdaparkinson.org/article/deep-brain-stimulation-and-swimming/ (Accessed: 26 October 2022).
‘Life after deep brain stimulation – eParkinsonPost’ (no date). Available at: https://parkinsonpost.com/life-after-deep-brain-stimulation/ (Accessed: 26 October 2022).
St. Joseph’s Hospital and Medical Center, Phoenix (2022) Exercise in Advanced Parkinson’s Disease (PD) With Deep Brain Stimulation (DBS). Clinical trial registration NCT05204680. clinicaltrials.gov. Available at: https://clinicaltrials.gov/ct2/show/NCT05204680 (Accessed: 25 October 2022).
What you need to know about deep brain stimulation (DBS) | News (2020). Available at: https://news.llu.edu/patient-care/what-you-need-know-about-deep-brain-stimulation-dbs (Accessed: 26 October 2022).


Books of Discovery: www.booksofdiscovery.com
Advanced-Trainings: www.advanced-trainings.com
About Til Luchau and Advanced-Trainings.com:
As a Certified Advanced Rolfer™, Til was on the faculty of the Dr. Ida Rolf Institute® for 20 years, where he served as Coordinator and Faculty Chair of the Foundations of Rolfing Structural Integration program. The author of the Advanced Myofascial Techniques textbook series (which has been translated into 6 languages), his regular Myofascial Techniques and Somatic Edge columns have been featured in Massage & Bodywork magazine since 2009, and (along with Whitney Lowe) he co-hosts the popular Thinking Practitioner Podcast. He is the Director of Advanced-Trainings.com which since 1985 has offered short, credit-approved professional trainings and certification for manual therapists of all types, in person and online.
Website: Advanced-Trainings.com
Email: info@advanced-trainings.com
Facebook: facebook.com/Advanced.Trainings1/
Instagram: instagram.com/tilluchau
YouTube: youtube.com/user/AdvancedTrainings
[music]
0:00:00.2 Ruth Werner: Join Til Luchau on a floating raft house in Thailand, surrounded by a jungle eco-preserve for 10 days of myofascial bodywork, Zoga movement and restorative learning starting February 20th, 2023. Or join Til for some powerful at-home learning with his monthly subscription, giving you unlimited access to more than 35 curated classes including advanced myofascial techniques, movement for bodyworkers, Feldenkrais and more. It's super affordable, and you can pause or cancel at any time. Sign up now at advancedtrainings.com.
[music]
0:00:41.7 RW: Hey, I Have a Client Who listeners, did you know I have a growing library of NCB-approved one-hour online self-paced continuing education courses that you can do any time, anywhere? Well, now you know. Current classes include, What's Next? COVID-19 Updates for Massage Therapists and A Massage Therapist's Introduction to Pharmacology Pt 1, and brand new, A Massage Therapist's Introduction to Pharmacology Pt 2. Classes are $20 each, and they confer one hour of continuing education credit. Wanna know more? Visit my website at ruthwerner.com and check it out. Be sure to sign up for my mailing list so you'll never miss a new class.
[music]
0:01:37.2 RW: Hi and welcome to I Have A Client Who, pathology conversations with Ruth Werner, the podcast where I will discuss your real life stories about clients with conditions that are perplexing or confusing. I'm Ruth Werner, author of A Massage Therapist's Guide to Pathology, and I have spent decades studying, writing about, and teaching about where massage therapy intersects with diseases and conditions that might limit our client's health. We almost always have something good to offer even with our most challenged clients, but we need to figure out a way to do that safely, effectively and within our scope of practice. And sometimes, as we have all learned, that is harder than it looks. Today's I Have a Client Who story comes from a massage therapist who got quite a surprise while they were working with their client's neck. And it goes like this, "Dear Ruth, I have a client who has a deep brain stimulation or DBS device. I'd met this gentleman at the franchise I work at a few days a week, and it wasn't mentioned in his previous SOAP notes or it slipped somebody's mind, I'm not sure, but you can imagine my surprise when I went to work on his lateral neck and felt either the tightest, thinest sternocleidomastoid I've ever palpated, or a bass guitar string under his skin."
0:03:04.9 RW: "Palpation plays such a huge role in what we do as therapists. And thankfully, my thumb felt this just as I was about to progress into an effleurage down and across his traps. He obviously picked up on how I went posterior to it and then palpated up and down, and finally he let the cat out of the bag about the device. It's like a pacemaker for his Parkinson's. The battery implanted in his chest and the cable runs along his SCM into his skull, delivering small electrical impulses. And he admitted that he somehow forgot to mention this. He had difficulty speaking at times, but it was definitely an interesting learning moment for me. I had no idea such a thing existed, never came across one with other patients who'd had Parkinson's. And as I read and learn more, apparently, DBS doesn't work for everyone, but for him, it seems to get the job done. He's used to it and says he's never had any issues. Have you ever come across this device?" Well, contributor, that must have been a shock. We could make this into an episode about the importance of good client intake forms so this kind of information gets communicated even in high traffic settings like spas or franchises, but let's not. Also, here is a long awaited I Have a Client Who story about someone with Parkinson's disease.
0:04:28.1 RW: But DBS is used for many conditions other than Parkinson's, so I'm gonna put Parkinson's off until I get a question with a more specific focus on that condition. So for today, let's turn our attention to deep brain stimulation devices because this is really cool. Parkinson's disease, essential tremor and dystonia, and we had an episode about dystonia quite recently. These are all movement disorders, they can involve tremors, that's arrhythmic oscillation of one or more parts of the body, usually on a single plane, or movement disorders can involve random choppy multi-plane muscle contractions. Tremors and contractions might be painful, they often interfere with basic activities of daily living. These disorders can also involve problems with muscle tone, this can look like rigidity in parts the body, especially in flexure, like the abdominal muscles and flexures of the upper extremities, and unsteady gait, and bradykinesia, technically that means slow movement. Brady means slow and kinesia, of course, is movement. But in practical application, we use the term bradykinesia to mean that it is really hard to initiate movement. People talk about feeling stuck or glued to the floor when they wanna move, and then that movement might be over-exaggerated because it takes so much effort once it begins.
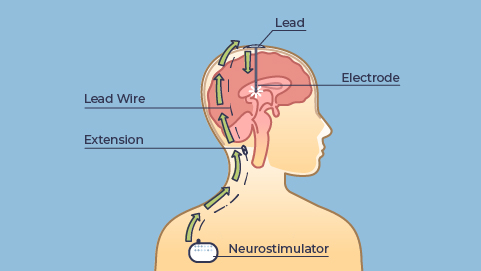
0:05:58.9 RW: You can imagine this is exhausting with tense, tight muscles, a high risk of falling and lots of other challenges. But what if we could send a controlled and targeted electrical impulse into exactly the parts of the brain that control these motor signals? Might that have a benefit for people who struggle with movement disorders? Those parts of the brain are highly localized and for brain anatomy nerds, and I confess, I am not yet a member of this club, I can tell you that we are talking about the subthalamic nucleus or the internal segment of the globus pallidus. So if we introduce a careful and controlled low voltage electrical current into these areas, will it suppress these involuntary muscle contractions and normalize movement? Turns out, yes, sometimes. Deep brain stimulation or DBS is a procedure to help with movement disorders and maybe a few other things, we'll talk about that just a bit at the end, by implanting electrodes into the correct portions of the brain and then running a wire down the neck to a pulse generator that is implanted just inferior to the clavicle, and then the current is adjusted so that the stimulating electrodes can help to organize these previously disorganized signals coming out of motor control centers. At least, that's the theory.
0:07:36.5 RW: Interestingly, the science about how DBS specifically works, not completely settled. And you have to wonder, who thought that would be a good idea? Well, the concept of stimulating the cerebral cortex with electricity goes way back, Frankenstein, or The Modern Prometheus, was published in 1818, for context, but the first human cortical stimulation happened in 1874. And then we used this technique to help map out the cortex and its functions. But electrical stimulation specifically targeted for movement disorders didn't come into use until 1980, so it's a relatively new intervention. We see that DBS improves the situation with movement disorders for lots of patients. About 160,000 DBS devices have been implanted so far, and about 12,000 procedures are performed each year to implant new ones. And as the technology improves with smaller devices and safer surgeries and longer lasting batteries, we will probably see this intervention become more common in coming years, especially since we might find some new applications for it. Getting a DBS device is not simple or quick. It requires a great deal of testing and at least two surgeries. The first surgery is the implantation of the leads into the brain, which involves drilling into the skull and then communicating with the patient to establish the correct placement.
0:09:13.2 RW: Then the pulse generator is placed under the skin below the clavicle and is connected by an extension wire under the skin in the neck to the electrodes in the brain. During follow-up care, the placement is confirmed to make sure it's in the right spot, and the pulse generator is programmed by way of a wireless built-in antenna, and this can be adjusted if the disease or the condition progresses, and of course, that's a big help. So I hope you're getting the picture that this is a complicated and intrusive procedure. The surgery-related risks are fairly low, but pretty serious including infection and sepsis, bleeding, stroke and coma. And once the device is implanted, calibration is sometimes challenging. Some patients report dizziness and balance problems and double vision and numbness or tingling in different parts of the body, sometimes even seizures or sudden weakness where all the muscle tone just disappears. And a lot of this goes away as the body adjusts to this new equipment, but clearly this is not something to be undertaken lightly. DBS is not the answer for every person with a movement disorder. Traditionally, it's been recommended as a last-ditch option for people whose situations didn't respond to medication, but more current recommendations suggest that it could be useful even when medications also improve symptoms, but just not enough.
0:10:44.6 RW: Certainly, it's not an either or decision. DBS is not a substitute for medication to manage movement disorders. Let's return to the client in today's story, again, here's what our contributor offered, "You can imagine my surprise when I went to work on his lateral neck and felt either the tightest, thinest sternocleidomastoid I've ever palpated or a bass guitar string under the skin. Palpation plays a huge role in what we do as therapists. And thankfully, my thumb felt this just as I was about to progress into an effleurage down and across his traps. He obviously picked up on how I went posterior to it and then palpated up and down, finally, he let the cat out of the bag about this device. It's like a pacemaker for his Parkinson's. The battery was implanted in his chest, the cable runs along his SCM into his skull and it delivers small electrical impulses." Okay, so now you know a little more about DBS devices and how they work and all the things that are involved with them. So I'd like to ask you what kinds of follow-up questions might you have for this client? Think about that for a moment. And here are a few I came up with, how long ago did you have this procedure? For instance, I would suggest waiting until the surgeries are completed and the calibration of stimulation is sorted out before doing anything rigorous with bodywork.
0:12:11.6 RW: I might also ask, do you have any lingering problems with it, like dizziness or numbness or other complications? Is it comfortable for you to be face-down on the table or have pressure on your neck? Is it comfortable for you to exercise and what does your exercising look like? And if you like the answers, then it's hard to see a reason not to proceed with massage. I tried to find documentation of any long-term restrictions with DBS devices, like we might see with a cerebral shunt for instance, and I didn't find anything. I also looked up what kinds of physical limitations people with DBS devices might have, and I didn't find much there either, except one really odd side effect. A number of people with Parkinson's disease found that after their DBS procedure, they could no longer swim. Not because of water and an electrical device, but because somehow they had simply lost the ability to coordinate their muscles, and before their procedure they had been competent swimmers. It's not true for everyone, but it is surely an interesting finding, and now people who have DBS devices inserted are advised not to swim on their own, just in case they have a problem. But I couldn't find any other issues with activities, and in fact, I did run across one clinical trial that is currently recruiting participants to look at aerobic exercise for patients with DBS devices.
0:13:35.7 RW: So I'm inclined to say that massage therapy is probably safe too. If you have clients who have undergone a DBS procedure or are considering it, I recommend that you check out the resources in today's show notes. I found a Creative Commons x-ray of a person's brain with the electrodes in place. I also found a newsletter from a Parkinson's support group in Canada, in which a couple of patients shared their DBS experiences, and that's a really great way to get a sense of how this treatment can affect a person's life. Right now, deep brain stimulation is an accepted intervention for certain patients with Parkinson's disease, dystonia and essential tremor. A few cases of deep brain stimulation for Tourette's syndrome have been published, and DBS for intractable pain situations like cluster headaches and phantom limb pain appear to offer some benefit, although these haven't yet been studied in great detail. But we are also looking at DBS for some other issues. It could end up being an option for people with medication-resistant obsessive-compulsive disorder and depression and even eating disorders or addiction. I'm interested to see where this goes, but to tell you the truth, I'm a little nervous about it. I'm having a hard time pinning down exactly why, but it seems like the potential for things to go wrong with an intervention like this is pretty high.
0:15:01.9 RW: But for the moment, let's celebrate how much better life is for people with movement disorders who have had successful DBS procedures. Hey everybody, thanks for listening to I Have Client Who pathology conversations with Ruth Werner. Remember, you can send me your I Have a Client Who stories to ihaveaclientwho@abmp.com. That's ihaveaclientwho, all one word, all lower case, @abmp.com. I can't wait to see what you send me, and I'll see you next time.





