10/20/2023
A client with a 3-week-old pacemaker wants a relaxation massage. Her Facebook group of other pacemaker users encourages her to do it, but her massage therapist is hesitant. When exactly is it safe for this person to get on a massage table?
Spoiler alert: No one knows for sure, but we can make some pretty confident choices, and we go over those choices on this episode of “I Have a Client Who . . .”
Resources:
Pocket Pathology: https://www.abmp.com/abmp-pocket-pathology-app
Clients with Medical Implants (no date). Available at: https://www.abmp.com/textonlymags/article.php?article=790 (Accessed: 18 October 2023).
Digby, G.C. et al. (2009) ‘Physiotherapy and cardiac rhythm devices: a review of the current scope of practice’, Europace: European Pacing, Arrhythmias, and Cardiac Electrophysiology: Journal of the Working Groups on Cardiac Pacing, Arrhythmias, and Cardiac Cellular Electrophysiology of the European Society of Cardiology, 11(7), pp. 850–859. Available at: https://doi.org/10.1093/europace/eup102.
Pacemaker (for the Heart): Surgery, Types & What It Is (no date) Cleveland Clinic. Available at: https://my.clevelandclinic.org/health/treatments/17360-permanent-pacemaker (Accessed: 18 October 2023).
Pacemaker Insertion (2021). Available at: https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/pacemaker-insertion (Accessed: 18 October 2023).
Pacemakers - Who Needs Them | NHLBI, NIH (2022). Available at: https://www.nhlbi.nih.gov/health/pacemakers/who-needs (Accessed: 18 October 2023).
Q&A: Novel Therapy Holds Promise for Hypertension Treatment in Patients With Pacemakers (2023) AJMC. Available at: https://www.ajmc.com/view/q-a-novel-therapy-holds-promise-for-hypertension-treatment-in-patients-with-pacemakers (Accessed: 18 October 2023).
Sabin, G. and Schuster, P. (1982) ‘[Long-term observation of arterial blood pressure after pacemaker implantation (author’s transl)]’, Deutsche Medizinische Wochenschrift (1946), 107(15), pp. 575–578. Available at: https://doi.org/10.1055/s-2008-1069979.


0:00:00.0 Ruth Werner: Hello, I Have a Client Who listeners. Ruth Werner here and I'm so excited to let you know that my library of online self-paced continuing education courses has just expanded. I now have a 2-hour ethics course called A Doctor's Note is Not Good Enough... And What is Better. This NCB TMB approved course goes into why a doctor's permission or approval or even a prescription doesn't provide the legal or safety protection you might think it does. Then we look at how to start useful conversations with health care providers that will actually get us to safe and effective massage for our clients with complex conditions. Visit my website at ruthwerner.com for more information and to register for A Doctor's Note is Not Good Enough... And What is Better.
[music]
0:01:00.1 RW: Hi and welcome to I Have a Client Who, pathology conversations with Ruth Werner, the podcast where I will discuss your real-life stories about clients with conditions that are perplexing or confusing. I'm Ruth Werner, author of A Massage Therapist's Guide to Pathology, and I have spent decades studying, writing about, and teaching about where massage therapy intersects with diseases and conditions that might limit our clients health. We almost always have something good to offer even with our most challenged clients, but we need to figure out a way to do that safely, effectively, and within our scope of practice. And sometimes, as we have all learned, that is harder than it looks.
0:01:46.2 RW: Today's I Have a Client Who is on a topic I'm a little surprised we haven't covered here before, working with clients who have pacemakers. Specifically, in this case, a newly installed pacemaker, which makes this decision a little more complicated. I'm going to share this story with you and then provide a little background information on these devices, and then we can evaluate our contributor's decision. They wrote me this letter.
0:02:13.7 RW: "Hi Ruth, my name is Redacted. I'm hoping to pick your brain about the timing of safe massage with new pacemakers. I have a 73-year-old female client who just had a pacemaker put in three weeks ago. I've only seen her once before so I don't really know her body or her personality well, but apparently, she's feeling good and she's very eager to book a relaxation massage with me. For starters, I asked what restrictions her doctor has for her and she texted, 'At present I have restrictions against moving my entire left arm directly above my head or lifting anything over 10 pounds for six weeks after the surgery. It's now been three weeks.' She went on to say, 'At this point, I could really use some work on my back and neck and feet. I think energy work would be great on my shoulders and arms. I'm still having high blood pressure issues and I think massage helps that.'"
0:03:10.9 RW: This is our therapist again. They said, "I found a 2014 ABMP article by you titled, Clients with Medical Implants. Understanding Some Common Devices." And here, this is Ruth now, and of course, I will put a link to this article in our show notes. And our contributor goes on, "In the article you say, pacemakers that have been in place for more than a few months pose no specific cautions for massage as long as the client is comfortable on the table. And that's helpful to know, but my question is, what about newer pacemakers that have not been in place that long? How long should I be waiting before doing anything that involves her laying prone, or when is it safe even to do gentle work to her upper back or anywhere near her neck or shoulders or arms?
0:03:54.9 RW: And just to complicate matters, apparently this client has joined a Women with Pacemakers Facebook group and she posted a question about massage and now she's telling me about all these Facebook responses saying, 'Yes, go get a massage.' I roll as if that's all the criteria I need to make a safe and responsible decision about how and when to massage her. So I guess I'm actually asking you for help on two fronts. Number one, timing. At what point post pacemaker surgery is it safe or not safe to do what exactly? And two, how do I explain professionally and succinctly why I need to be cautious, what the main concerns are in this case, and why I'm needing to gather more clinical information than what her Facebook friends are telling her?"
0:04:44.8 RW: Yeah, that's all one big question swirling around in my head, and I have to say, this massage therapist is singing my song. And I sent them a quick reply. I said, "Your question about restrictions was spot on. It would be good to know about her meds and side effects and daily activities too." And here's what I got back. Our therapist said, "For your information, my entire practice is built on helping my clients decompress. I do this by softening and loosening muscle tension and soothing the nervous system. In other words, it's a customized, slow paced, feel good massage. I don't claim to or have any desire to treat pain or injuries or offer deep tissue work. That's all to explain that I am not used to dealing with more medical questions like this, and so it has instantly made me feel uncomfortable and incompetent.
0:05:40.7 RW: And the client had provided more information as well. The client says, "At the moment, my blood pressure medications are in a state of flux. The cardiologist and I are trying to find the right dosage that will control the blood pressure adequately. The reason for the pacemaker is so the dosage of blood pressure medication can be increased without lowering my heart rate." And then the client shared some details about her meds that I won't go into. And they said, "As for the doctor issuing a clearance for daily activities, those actual words were not used in our consultations. But the written instructions I received say that, number one, implant patients are are okay to drive and resume normal showering after one week. Two, at four weeks, if the bandage hasn't fallen off, we can take it off. Three, we are not to raise our arm above shoulder level or stretch it behind our back for four weeks. Four, no lifting anything over 10 pounds for six weeks. Five, no vigorous exercise for six weeks. And six, no contact sports or swimming or golf for 12 weeks.
0:06:51.0 RW: That would all seem to me to imply that normal activities are fine at six weeks and I will be at four weeks this coming Tuesday. I'm already doing normal activities so long as they don't involve lifting over 10 pounds or raising my left arm above my head. I have been driving, cooking, cleaning, shopping, carrying and putting away groceries, sewing, doing laundry, blowing leaves, raking black walnuts, washing windows and scraping and painting doors. I've also used small tools on projects like a saw, hammer, screwdriver, drill, chisel and so on. I could say I've been doing normal activities for at least two weeks. At my last appointment with my cardiologist, he asked me to have my primary care physician set up an appointment with a physical therapist to start doing post surgery exercises. My next appointment with him is in a month to check on the blood pressure medication results. There are no issues or problems with the pacemaker."
0:07:45.6 RW: And our contributor concludes, "I think I'll just tell my client I'm not comfortable massaging this soon and book her a few weeks out. And then if I learn anything new, I can adjust the timing as appropriate."
0:07:58.0 RW: Well, my goodness, this is amazing. How often do you get this much information to feed into your clinical decision making? But before we can make any judgments about the safety of massage therapy for this client, we need to learn just a bit about pacemakers. And I used some of my favorite resources for this; Johns Hopkins University, the National Institutes for Health and the Cleveland Clinic, but truthfully, this information is really well established, and essentially, you will find the same information wherever you look. I'm sure you're aware that your heart has its own electrical generator and impulse system that allows its fibers to contract in a highly complex and coordinated pattern. And that pattern makes constant adjustments in speed and intensity, depending on your needs from moment to moment. When there are problems with the electrical impulses in the heart, maybe because of a previous heart attack that damaged that portion of the myocardium, then a pacemaker may be installed.
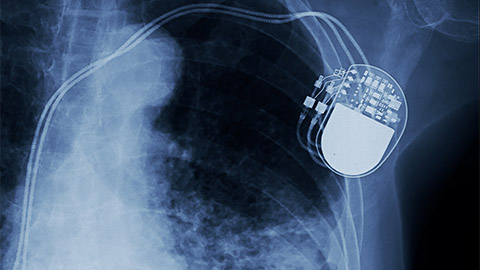
0:09:01.5 RW: But our client in today's story didn't say anything about a history of a heart attack. Huh? Does she really need a pacemaker? Well, we'll get back to that in a moment. Pacemakers have been around for decades. About 350,000 Americans get one every year, and they come in three main varieties. There's one that's implanted directly into the heart muscles with no wires or pulse generator; and there's one with a pulse generator just under the skin on the chest that's connected to a single insulated wire that's called a lead and that lead connects to the targeted ventricle with an electrode; and there's a version with two leads going to whichever chambers need to be reorganized. During the insertion procedure, the leads are threaded through an artery or a vein to reach the right section of the heart. Both of these types of pacemakers involve a pulse generator that is located just under the skin below the clavicle. This is where the pacemaker battery is located. And those batteries last for 10-15 years, and replacing them is fairly simple.
0:10:08.0 RW: After a few months, scar tissue grows all around the leads and makes them extremely stable. They really don't budge. And that's why the common wisdom is that massage or sports or other activities are safe at this point. Getting a pacemaker is not risk free, as you can imagine. People can develop blood clots, they can have blood vessel damage or infections, sometimes much more serious complications come up, they're pretty rare. There's also a situation called pacemaker syndrome, where doctors are unable to establish good coordination of the heart muscle regardless of how the device is used. Also, a person with a pacemaker can't receive an MRI, they might set off metal detectors at the airport, and they have to avoid having any magnets near their chest.
0:10:55.1 RW: So a lot of people with a history of heart attack end up with a pacemaker. But that is not the situation with our client. And it turns out that lots of people can benefit from a pacemaker even without a history of a heart attack. A person with arrhythmia that can't be managed with medication is a good candidate. A person with heart failure where the organ just gets weaker and weaker might need one. And interestingly, a person with hard to control high blood pressure can benefit from a pacemaker, and that describes the client in this story. One of the articles I read to prepare for this episode went into some details about the challenges of managing the blood pressure of older people, and I'm telling you, it was fascinating. Balancing the right amount of cardiac force versus resistance with the body's tendency to compensate by constricting peripheral arteries, sometimes in some unhelpful ways, it just really opened my eyes up to this challenge.
0:11:56.7 RW: So let's come back to our story. Here is this 73-year-old woman, and her health care team has not been able to get on top of her hypertension, and that puts her at risk for atherosclerosis and heart attack and stroke and all kinds of horrible things. So, in order to give her the right combinations and doses of medications that she needs to both protect her heart and to compensate appropriately with the rest of her cardiovascular system, she had a pacemaker inserted, which sounds like a good strategy. This is a person who is clearly fit and active. It sounds like, just a few weeks after this procedure, she's already more active than I am with her paint scraping and tool using and leaf blowing and so on. And we have a really full and thoughtful list of her guidelines on daily activities, and she's getting ready to add physical therapy. And in general, it just sounds like she has some soreness, but her recovery is going well.
0:12:57.5 RW: Remember, these are her words. "At this point, I could really use some work on my back and neck and feet. I think energy work would be great on my arms and shoulders. I'm still having high blood pressure issues, and I think massage helps that." Now, let's review our contributors description of their work. They say, "For your information, my entire practice is built on helping my clients decompress. I do this by softening and loosening muscle tension and soothing the nervous system. In other words, it's a customized, slow paced, feel good massage. And this is all to explain that I'm not used to dealing with more medical questions like this, so it instantly has me feeling uncomfortable and incompetent."
0:13:45.6 RW: Well, between these two people, the client and the therapist, boy, there's a lot to unpack here. But I'm just gonna focus on a few little things. One is, humility is a very good thing, and I applaud this massage therapist for their caution and their desire to be safe, and they're feeling like they want more information. And I also want to encourage this massage therapist to understand that this trait makes you more competent, not less competent. Also, people with complex medical situations, like this client, seek massage, even or especially from therapists who specialize in relaxation work, which by the way, is the very hardest kind of massage to offer, in my opinion.
0:14:31.6 RW: Our contributor asks these very good, very specific questions. Timing. At what point post pacemaker surgery is it safe or not safe to do what exactly in terms of massage? [laughter] Nobody knows. I looked up what I could find. I found a single paper on physical therapy for people who had recently gotten a pacemaker, and the conclusion was essentially we don't know when it's safe for sure, so just go slow for a while. That's helpful, right? And the second question is, how do I explain professionally and succinctly why I need to be cautious, what the main concerns are in this case, and why I'm needing to gather more clinical information than what her Facebook friends are telling her?
0:15:22.8 RW: Well, I think you've nailed it here. You could use language like, "There's no reliable information on massage for someone with a recently implanted pacemaker. So for your safety, I want to err on the side of caution. And after you've been moving and working with this device for a few weeks, let's try some gentle massage and see how it goes. I'm cautious about whether you'll be comfortable face down on the table because of this device on your chest, and I'm cautious about disrupting the leads because they have not yet really been fully seated with scar tissue. We also might want to do shorter sessions to begin with so that we can make sure that you're as comfortable as possible."
0:16:06.4 RW: Okay. Now, listeners, given what our client has been through, can you think of an approach to bodywork that is a better match for her than what this massage therapist offers? I think this contributor will do great things with this client who seems to me like just an amazing person. I wish I'd been able to respond more quickly to this contributor's letter.





